Past Research Studies
|
Mobile Alcohol Response Study (MARS)
MARS evaluates the effects of alcohol consumption and smoking in a natural environment on mood, behavior, and other related experiences. Chicago STOP Smoking Research Project (C-STOP)
This study examines the efficacy of an FDA-approved smoking cessation medication in combination with standard treatment of nicotine patch and behavioral counseling in a sample of adults who drink alcohol and want to quit smoking. See below for publications: Chicago Community Health Study (CCHS)
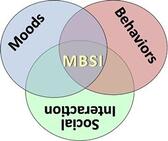
This study examined how community members in the Chicago area who previously participated in the Chicago Multiethnic Prevention and Surveillance Study (COMPASS) respond to information and health feedback on health, smoking, and related activities. Enrollment for this study is complete. Moods, Behaviors, and Social Interaction Project (MBSI)
The MBSI Project examines moods and behaviors in response to common tasks and social interaction in a young adults with a variety of drinking and smoking patterns. |
Chicago Community Health Study (CCHS)
For this study, 204 smokers from the University of Chicago COMPASS trial who identified as Black/African American were randomized to Enhanced Care (30-minute culturally-targeted, motivational counseling session and one- week nicotine replacement kits, along with pamphlets and self-help materials) or Treatment As Usual (self-help materials only).
Average age was 54 years and half of participants were female. Two-thirds of participants completed a high school education but three-fourths were not currently employed. On average, participants smoked 8.8 cigarettes per day with 96% reporting menthol cigarette use.
Results showed that participants who received enhanced care gained a better understanding of nicotine replacement therapy and their benefits. One month later, Enhanced Care participants reported, on average, a much greater reduction in cigarettes smoked per day (43% reduction vs. 13% reduction) and were more likely to use nicotine replacement for behavior change than those receiving usual care (58% vs 8%). Current analyses are examining the effects of in-session sampling of nicotine replacement in enhanced care and whether self-report of smoking reduction is confirmed by two tobacco-specific biomarkers, including cotinine and 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol (NNAL).
The study showed that Black smokers who are primarily low-income and not seeking treatment can make important behavior changes as a result of targeted motivational counseling and making use of nicotine replacement convenient and accessible.
Average age was 54 years and half of participants were female. Two-thirds of participants completed a high school education but three-fourths were not currently employed. On average, participants smoked 8.8 cigarettes per day with 96% reporting menthol cigarette use.
Results showed that participants who received enhanced care gained a better understanding of nicotine replacement therapy and their benefits. One month later, Enhanced Care participants reported, on average, a much greater reduction in cigarettes smoked per day (43% reduction vs. 13% reduction) and were more likely to use nicotine replacement for behavior change than those receiving usual care (58% vs 8%). Current analyses are examining the effects of in-session sampling of nicotine replacement in enhanced care and whether self-report of smoking reduction is confirmed by two tobacco-specific biomarkers, including cotinine and 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol (NNAL).
The study showed that Black smokers who are primarily low-income and not seeking treatment can make important behavior changes as a result of targeted motivational counseling and making use of nicotine replacement convenient and accessible.
Chicago STOP Smoking Research Project
122 smokers with heavy drinking patterns and motivation to quit smoking were recruited to participate in this double-blind, placebo-controlled research study. 61 participants were randomly assigned to receive both varenicline and nicotine patches, while 61 participants received placebo and nicotine patches. Participants were 44 years old on average, 54% non-white, 45% female, drank an average of 5.7 drinks on drinking days, and smoked an average of 12 cigarettes per day.
At 9-12 weeks after participants' quit date, 27 participants (44%) reported abstinence in the varenicline group while 17 participants (28%) reported abstinence in the placebo group. These results suggest that, for smokers with heavy drinking patterns, combined treatment with varenicline and nicotine patch was more effective than placebo and nicotine patch for smoking cessation.
At 9-12 weeks after participants' quit date, 27 participants (44%) reported abstinence in the varenicline group while 17 participants (28%) reported abstinence in the placebo group. These results suggest that, for smokers with heavy drinking patterns, combined treatment with varenicline and nicotine patch was more effective than placebo and nicotine patch for smoking cessation.